Tuberculosis (TB): Background, Pathophysiology, Etiology


Health equity can be achieved only when every person has the opportunity to reach their full health potential, regardless of social, economic, or environmental circumstances.
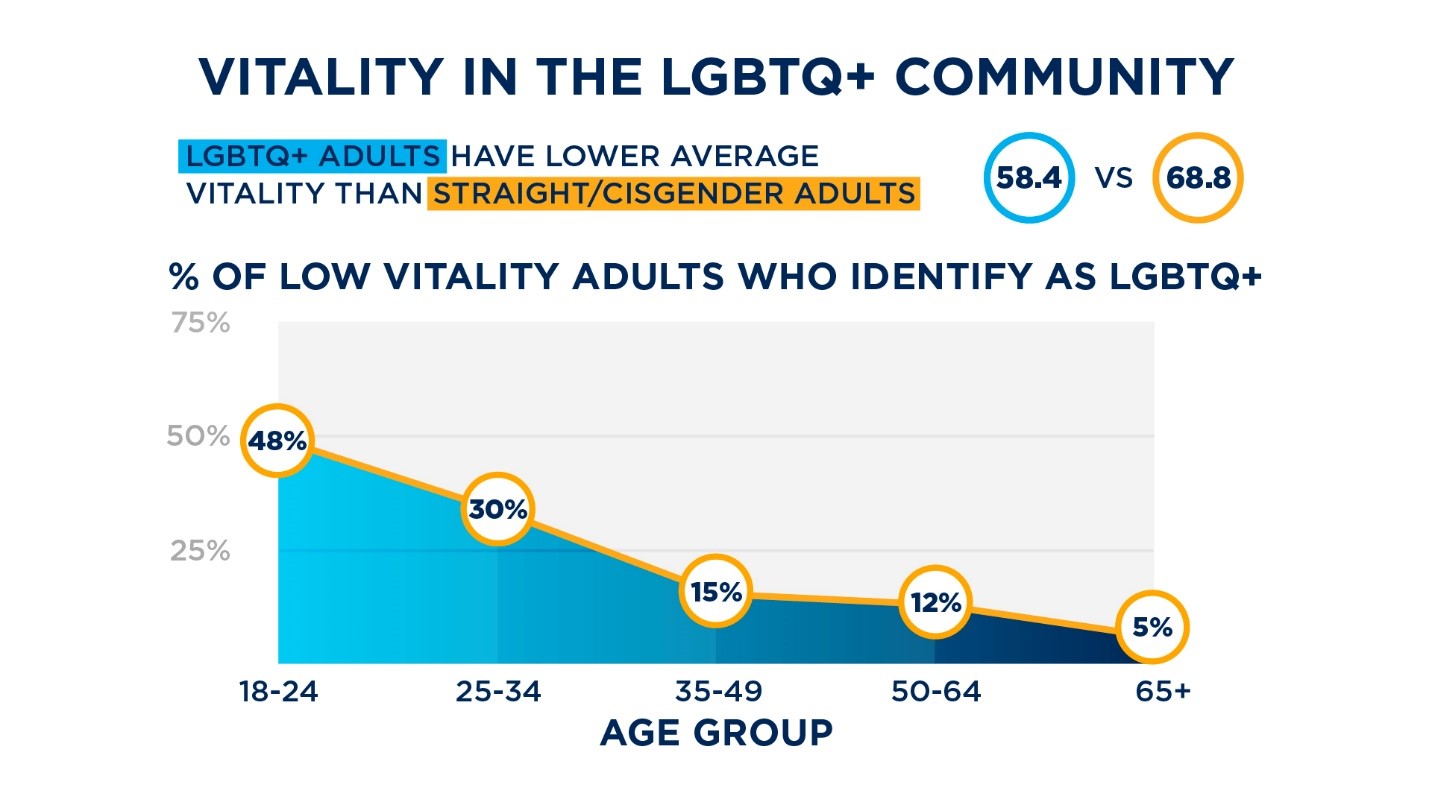
But the hard truth is that today, health equity is nothing more than an aspiration – particularly within the LGBTQ+ community. LGBTQ+ people are at higher risk for suicide and suicidal thoughts, mood disorders and anxiety, eating disorders, alcohol and substance abuse, and tobacco use. LGBTQ+ people also have less access to health care and have worse health outcomes.
Recent research from Cigna Corporation, which surveyed 10,000 U.S. adults to better understand their vitality levels, finds that the LGBTQ+ community faces barriers in finding health care providers who are culturally trained and sensitive to their health needs. For example, 50% of LGBTQ+ individuals strongly feel their provider really listens to them, compared to 63% of heterosexual, cisgender individuals. Also, 49% of LGBTQ+ individuals strongly feel respected by their provider, compared to 62% of heterosexual, cisgender individuals. The trend continues with 51% of LGBTQ+ individuals reporting strong feelings of trust in their provider, compared to 65% of heterosexual, cisgender individuals.
 We sat down with Dr. Renee McLaughlin, national medical director for LGBTQ+ health and well-being at Cigna, to talk through some of the health disparities LGBTQ+ people face, what causes these disparities, and how providers can help reduce the stigma and discrimination this community faces. Dr. McLaughlin also shared tips for providers on how to provide quality and inclusive care for LGBTQ+ people.
We sat down with Dr. Renee McLaughlin, national medical director for LGBTQ+ health and well-being at Cigna, to talk through some of the health disparities LGBTQ+ people face, what causes these disparities, and how providers can help reduce the stigma and discrimination this community faces. Dr. McLaughlin also shared tips for providers on how to provide quality and inclusive care for LGBTQ+ people.
The biggest barrier for LGBTQ+ people is finding providers in their local network who are culturally trained and sensitive, as well as clinically trained and competent in supporting the health needs of this community. LGBTQ+ people often feel discriminated against in their health care experience, which ultimately discourages them from seeking care when they need it.
It's twofold. First, while we are seeing an increase in the number of medical schools that incorporate LGBTQ+ health into their curriculum, health care providers don't have much training specific to the needs of this community. A study by the Association of American Medical Colleges found that most schools do include some LGBTQ+ coursework, but half reported just three or fewer lectures, group discussions, or other learning activities on this topic. Think about that: A 40-hour school week totals about 8,000 hours of medical education (in four years of medical school), and in that timeframe, medical trainees are only exposed to three lectures or so on LGBTQ+ health.
In addition to that, there are also cultural inhibitions (prejudice, discrimination, stereotyping, etc.) in supporting this community. Transgender people, in particular, have experienced discrimination in accessing health care, and that has translated into a reluctance to seek health care. One study found that nearly half of transgender people have been mistreated by medical providers, and 28% postponed or avoided necessary medical care for fear of discrimination.
While it may seem like the health needs of LGBTQ+ people would be largely the same as everyone else, there are some unique needs. For example, we know that there's a higher instance of substance use disorder as well as alcohol use in this community. We also know that there's often a higher burden of mental health. Just as we know that osteoarthritis is more common among women than men, providers need to keep in mind the health risks that the LGBTQ+ community faces as well.
The good news is there are a lot of resources. A good place to start is really understanding the cultural barriers and challenges in the health care environment for LGBTQ+ people. The Human Rights Campaign has a lot of really good literature, as does the GLMA (formerly known as the Gay and Lesbian Medical Association) and the World Professional Association for Transgender Health. There are also a few academic institutions that have a good LGBTQ+ health curriculum. The Fenway Institute in Boston, for example, has an excellent manual for lesbian, gay, bisexual, and transgender health.
When a patient is looking for an orthopedic surgeon, almost every practice is what we call "board certified," and that can be independently verified. The same holds true for almost every other medical specialist. This type of accreditation doesn't exist for LGBTQ+ health.
As a health plan, we recently took a step to improve the health care experience for LGBTQ+ Cigna customers by updating our online provider directories on myCigna.com to display providers who self-identify with the Council for Affordable Quality Healthcare as interested and experienced in caring for LGBTQ+ patients. This self-identification process brings business differentiation to providers and a better experience to patients.
Now, some might think that self-identification isn't necessary and that doctors need to treat all patients in the same manner, but that's not actually correct. You don't treat a diabetic the same as you treat someone with hypertension. They're different clinical scenarios and you treat them differently. Additionally, it is important for providers to understand the subtle differences in patients that can make a huge difference in outcomes.
Outside of enabling self-identification on myCigna.com, Cigna has developed specific training on LGBTQ+ health issues for over 600 Cigna clinicians, and resources are available to all in-network health providers on the Cigna website.
Doctors need to do everything they can to understand their patients and the full context of each individual's life. For example, the trans population sees a much higher rate of unemployment and housing issues – and understanding that context can help providers intervene appropriately. Additionally, providers need to stay up to date on culturally sensitive terminology. For example, what does lesbian mean? What is queer? What is transgender? Nonbinary? Education is key to inclusion.
Providers must think about the end-to-end care experience – everything from intake to respecting pronouns, preferred names, and more. I'm trans myself, and I'm in the midst of my transition. I have had experiences where I'm sitting in a doctor's waiting room for necessary care and I present as female, and the receptionist will shout out my male gender name to call me even though she has my preferred name on file. The health care experience starts way before the patient even sees the doctor. Everyone who interacts with a patient creates that environment where patients feel comfortable. And by the way, even if my doctor does end up providing me with competent care, having an awful experience with the front-end staff could keep me from visiting that office again. Building trust and a safe space will mean training staff on the appropriate ways to interact with LGBTQ+ people.
We need to empower members of the LGBTQ+ community to feel comfortable and motivated to seek care and to feel like they can have an open dialogue with their health care team. If I am a trans-identified male but still have my cervix and I go to the emergency room with lower stomach pain, the doctors there need to know that information in order to make an accurate diagnosis. It is possible that this pain could be a ruptured ovarian cyst, and it may be necessary to request a cervical cancer screening. That's just one example, and there are many more.
Comments
Post a Comment